On the Tuesday before Thanksgiving, the Rehab Center Medical Director told me that he wanted to release my mom by December 1st, ushering in another mad dash to figure out what to do. Before I left Mom that morning, I started calling the assisted living facilities in the Richmond area. I would have to find a place and move her in just over a week. And that week included the Thanksgiving holiday.
I toured five facilities and decided where she would move the following Monday. Bolstered by the experience at the Rehab center, I came to each tour armed with better questions and a more critical eye. Medicare does not cover Assisted Living so the cost would come from my mom’s savings this time.
I returned from each tour with brochures for Mom and gave her my observations. She wanted to go home and wasn’t asking too many questions. My sister contemplated quitting her job and moving mom into her living room on the first floor, but that was nixed by my mom immediately. My mom lived in a one-bedroom condo, making caring for her in her home difficult and expensive. Even with my sister and I taking as many hours as possible, the cost of in-home care would deplete her savings quickly, and she was adamant that I save as much as possible to give to her children. When I would tell her my job was to take care of her and not my siblings, she would muster up a curt response of “I’m not dead yet!” meaning she wanted me to do what she wanted me to do. My job was to thread the needle between quality of care and affordability.
As I toured the facilities that Thanksgiving week, in addition to cleanliness, I noticed how the staff interacted with the residents. Were they engaged? Did they look people in the eye? Were they kind? Did they look up from what they were doing when I entered their building?
I also looked at their uniform shirts, having learned that it could indicate the level of care. Were they clean? Did they fit? Did the staff seem invested in their jobs and the residents? Was the staff recognizable by residents and guests?
I wanted to know if there was always a manager on duty. From the Rehab Center, I learned that you need access to managers if a problem arises outside of normal business hours.
I tried interacting with the residents in each location to see if they seemed happy. I looked at the menus and the rooms to imagine how comfortable my mom would be in each location.
My sister was off the day of the last visit, and she went with me. The person giving us the tour seemed competent and nice. She knew the residents by name, which we liked. The facility seemed clean, but after learning from the rehab facility experience, we asked about the response time when a resident used the call bell. We were told approximately 30 minutes, which seemed long, but we appreciated the honesty. In the end, we didn’t consider this place, and here’s why: Each facility toured had either an empty room or a model to show us during the tour. Our guide at this place opened the door to a resident’s room and showed us around. We had met the resident earlier in the tour, so she knew he was downstairs, but the resident had not been expecting guests, so various personal items were visible. it felt like an extreme evasion of privacy to open the room to strangers. We crossed them off the list.
This experience made me think of all the businesses I have visited over the years and their level of preparation for my visit. Some had signs to welcome me. One company even made a personalized magnetic sign that covered the visitor parking sign for me. Others had swag, which was a nice touch. One of the travel coffee mugs I use almost daily was gifted during a client visit. Unfortunately, these examples are the exception to the rule. Most of my onsite visits would be classified as “not ready for guests.” Reception areas that rarely have a receptionist these days are usually covered in what can only be classified as “stuff.” Two large trashcans caught dripping water in the lunch room at one business I visited. Lights often flicker in the restroom, carpets often need to be replaced or, at least, professionally cleaned, and there is generally just too much clutter in the office area. Just like with the tour of the Assisted Living business, this is not putting your best foot forward for a customer or prospect visiting your facility. Today, businesses with this level of dishevelment will find it hard to recruit new talent. In addition, cluttered, unorganized spaces negatively impact employee engagement, lowering productivity and profitability.
My sister and I decided on the best place and shared our thoughts with Mom. The facility was about the same distance as the Rehab center for me, but it was just a few minutes from my sister’s home, which seemed helpful. The rehab facility was sapping Mom of her will to live, so when we made our final recommendation, Mom just nodded along. She wasn’t happy with the price, but she realized there weren’t a lot of options.
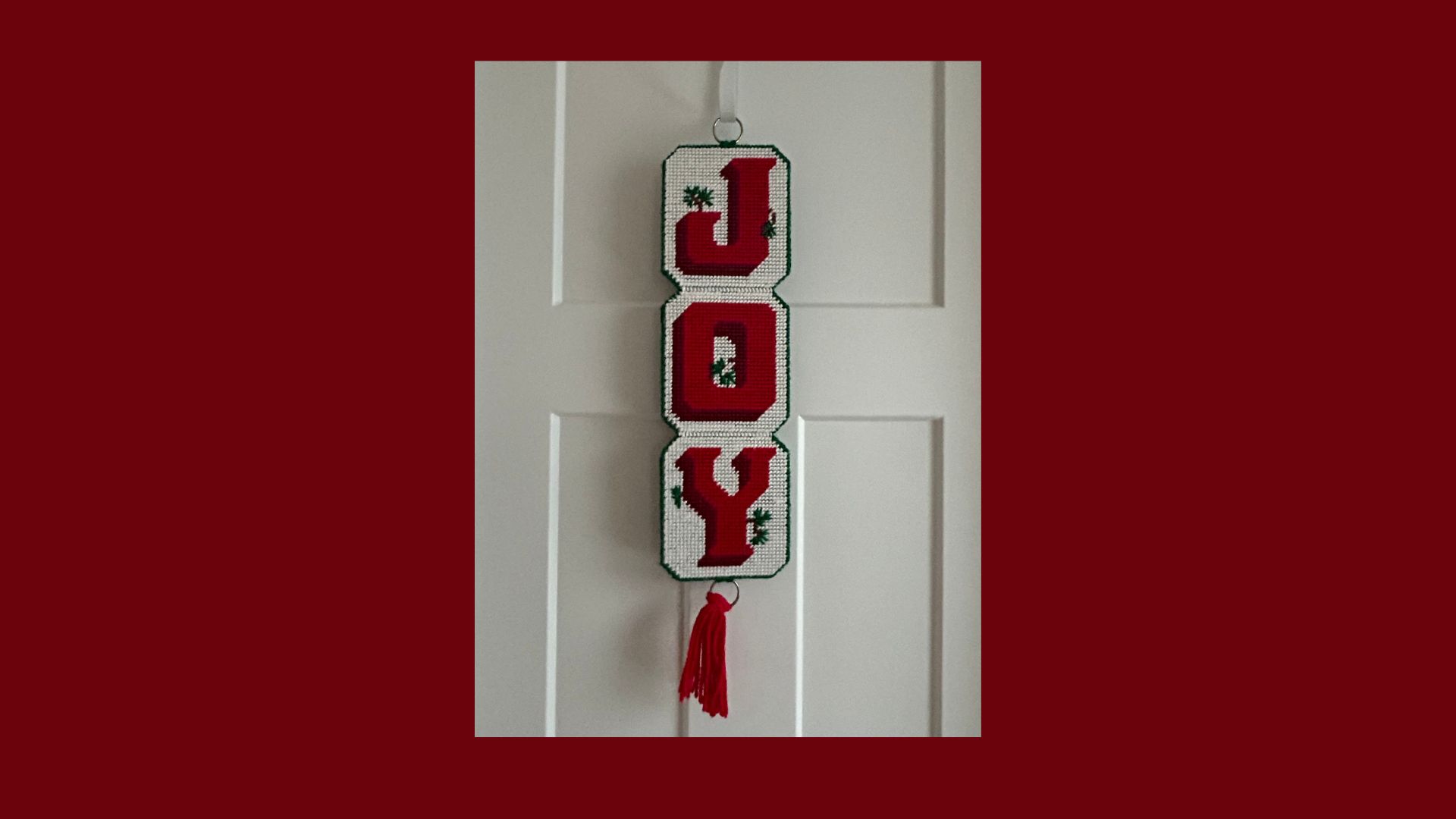
The move date was December 1st. The night before, a group of her children and grandchildren moved a few things from her condo to her new rehab studio apartment. We brought her favorite chair, a bedside table, and a lamp from her room at home. We also brought a few small touches to make her new room feel like home. The word “joy” was important to my mom’s faith and approach to life. We found a banner with the word “joy” that she used as a Christmas decoration and hung on the door to her new room. We also transported a little Christmas tree, a replica of their larger tree, which her husband made for her before he passed away years before.
On Friday, Dec 1st, I finished my day at noon and headed to pick her up and move her in. I couldn’t wait to get her out of the rehab facility. When I arrived, she told me that she had left a message for the facility director because she wanted to share some things before her departure. She said she wanted to make it better for future patients. In my head, I rolled my eyes. One of the aides told her that the director would be down “shortly.” My Mom waited in her wheelchair for almost an hour, but the nursing director never showed up. I knew she wouldn’t. When your culture is that bad, it’s broken at the top.
I finally convinced my mom that we should go. As I wheeled Mom out, we rolled past the nursing director, who could see that my mom was moving out. It would have been the perfect time to say, “I was on my way to your room.” She didn’t. She kept her head down, mumbled “hi,” and kept walking. For a second, I almost stopped so my mom would have the chance to “leave the place better than she found it.” I didn’t stop; I just wanted to leave because being there was just that bad. When your customers want to share something about their experience, even if you suspect it will be bad, you have to take the feedback. If you don’t, your culture will stay right where it is – bad. PS, today I received a bill for a haircut my mom got in November of 2023. They can even bill correctly.
Our arrival at assisted living was promising. A staff member was outside hanging holiday decorations. The center director came out to help me get my mom out of the car. I asked him to go up to her room and grab the wheelchair hospice had already delivered, so I could stay with mom. As he left I asked in a whisper if he could turn on the little Christmas tree so it would be on when she rolled in. When we opened the door to her room, the little Christmas tree was shining to welcome her. Things were happening like clockwork!
Hospice had delivered a hospital bed, so I quickly made the bed with the new linens I had purchased earlier and unpacked her suitcase. The room was clean and neat, and I was starting to feel like she would be comfortable there. The hospital bed had side rails, but these are not legal for assisted living, so the director was personally figuring out a solution that would give my mom some leverage to get in and out of bed. The director spent hours with us that day. My sister was there by this point, and we were very hopeful.
And then the bottom fell out.
The Hospice nurse showed up to confirm medications and ensure their equipment was set up properly. Several days before, I had sent the forms, including the medication list, to ensure it would be on hand, called to check and been told everything was on order. The med techs didn’t have them. Nobody seemed to know why they weren’t delivered or what to do about it. The hospice nurse stayed for several hours to help them figure it out. The nursing director showed up and got involved, and she couldn’t even determine why the medication order hadn’t originally gone through and wouldn’t go through now. My Mom needed Tylenol for pain in addition to her other medications, but it had not been delivered. I wanted to go to the drugstore and buy some. The Center director offered to go to the drugstore and get it, which he did. Hospice had the morphine so my mom wouldn’t be in pain, but all of the other medications were not there.
In the middle of all this, we tried the call bell. No one came. I worked on that problem while the others worked the phones to figure out the medication. Ultimately, it turned out that because my mom had arrived after 1:00 PM on a Friday, the new medication order had to be sent to the weekend pharmacy, not the regular pharmacy. The facility was part of the chain and used a common pharmacy two hours away. The mistake meant that the medicine would be delayed until the following day. The computer system did not alert the user that their order through the regular pharmacy would not be delivered and that they should use the weekend pharmacy. The people were trying, but the processes and systems let them down.
A similar situation occurred with the call bell. There was an amazing gal at the front desk whose job was to watch the call bell board and use a walkie-talkie to alert a person on the floor of the room number of the person needing assistance. This seemed like an ok plan until I realized each bell had to be reset after the resident activated it. If the staff member forgot to reset the bell, it would not work the next time it was pushed. This is nuts, but I fixed this by insisting that my mom be issued multiple call bells.
This seemed to solve the problem during the day but we were still having problems at night. Hospice wasn’t happy and wanted my mom to move to another facility. My mom liked the people, and she didn’t want to move. I had to get to the bottom of the call button debacle.
The next day, I went through the process with a fine-tooth comb and figured out what was happening. During the day, the receptionist monitored the call board and would page the staff to the appropriate room. After 8:00 PM, the calls were supposed to ring the pager of the floor lead, who would then use a walkie-talkie to alert the staff of the room needing assistance. It’s not the most technical solution I’ve ever heard, but it should work. But it wasn’t so that night; whenever I passed a staff member on the floor, I asked, “Do you have a pager.?” Do you have a walkie-talkie? Not a single staff member I talked to did.
The next morning, I marched into the Director’s office. He had only been working there for a month, and most of his focus had been on trying to fill staff vacancies, so he was learning a lot about his processes through our experiences. I shared that no one seemed to have a pager or a walkie-talkie at night. He told me that one of the first things he did when he arrived was buy a bunch of pagers and walkie-talkies. There were so many that the staff got careless about bringing them back in and would simply take another from inventory. It was news to him that the staff didn’t have them. I gave him a little free consulting and suggested that one set of pagers and walkie-talkies be turned over from one staff member to another at shift change so they never left the building. He could use the rest for backup when one malfunctioned. The next big problem would be to account for all of his inventory. But he was going to have to get them back or buy more because his process wouldn’t work at night if the staff didn’t have pagers and walkie-talkies.
Over the course of my career, I have seen big problems absorb owners’ attention, so much so that they don’t notice process errors that are costing them money and causing them to lose customers. In this case, the Director was fixated on filling the staff vacancies first before tackling the process issues under the surface. Staffing is critical, but his process issues might have been causing the staffing issues. Hiring good people and giving them a bad process will mean more turnover and more hiring and on and on. There will always be some major problems to draw an owner’s attention, but if owners don’t prioritize the systems and processes, they will always be swimming upstream.
One of the highlights of the experience was the dining and kitchen staff. The food was much better than the rehab facility. The servers knew each resident by name and served them like it was a restaurant. My mom liked all of them, especially the chef who made her a perfect over, easy egg every day. My husband was the only other person who got that high of marks on the egg front.
One day, I arrived to find that the entire dining and kitchen staff had gone on strike. None of them showed up for work. The nursing director and med techs made and served food when my mom arrived for breakfast. From the process side, that meant they weren’t doing what they were supposed to do, like ordering medication, for instance. This was another big problem for the facility Director to solve before dealing with his process issues. I don’t know the resolution, but everyone was back on duty by the lunch service.
One night before I left, my mom asked me for some paper. I ripped a few pages out of my notebook and gave it to her. When I came in the next day, she handed me a four-page plan to improve the facility. She documented everything she thought they could do better and the steps necessary to “right the ship,” as she liked to say. She told me she had called both the nursing and facility director and asked to meet to present her plan. She wasn’t going to wait until it was too late this time.
Her plan was pretty elaborate and even included advice for the director to take his wardrobe up a notch. Her plan said, “I’m not saying you have to wear a three-piece suit; I’m saying you have to look like you are in charge.”
Her plan called for the dining staff, which largely stayed the same day-to-day, unlike the med techs, to notice changes in each resident’s health. They were to alert the nursing staff if they noticed someone was failing. She had been noticing changes in the residents herself, especially a new friend who shared her table. She felt he was going downhill and asked him daily if he had been seen by the facility doctor. He had not she went to the staff herself to get him seen.
She had a whole section on unexplained noises that upset the residents needlessly. The noises were dragging trash cans and repeatedly opening and closing the doors on the medicine cart to pull medications. She recommended organizing the medicine by patient first so the cart only had to be opened once per patient. I wondered about this myself. It seemed like that cart was open and shut 15 times for each patient’s meds. Ultimately, she felt that everyone was working hard and cared, but their duties and processes weren’t organized well, resulting in frustrated employees and less than optimal care for residents.
My mom celebrated her 87th birthday on January 6th. We ate pizza and toasted with champagne in her room by the light of her little Christmas tree. Six days later, she was gone.
My mom was an amazing woman – way ahead of her time in many ways. In addition to being a wife and mother, she was a nurse, a realtor, a medical device sales rep, a small business owner, a funeral planning consultant, and a caregiver. She taught Sunday school, a lector at church, was on the parish council, and organized the prison ministry all in her eighties. Her church just notified me that they are presenting her with their Impact Award posthumously for helping to improve the parish.
My mom never met a problem she didn’t think she could fix and never failed to try. Making things better brought her joy. She wanted to leave every situation she found herself in better than the way she found it. She didn’t get the chance at the rehab center, so she made it a priority in her final days at the assisted living facility.
When she died, I got this email from the director of the assisted living facility:
“I enjoyed getting to know your mom. I am sorry things got off to a rocky start, and I appreciate everyone’s patience with us. She was a considerable help, and I learned quite a bit from her. I appreciate all the feedback she provided and will not soon forget her. We will keep working to address the issues she brought to light.
I really hope they did.
0 Comments